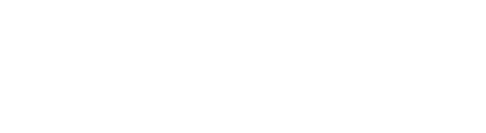
The Four Biggest Mistakes You Can Make After A Muscle Tear
July 17, 2019
THE FOUR BIGGEST MISTAKES YOU CAN MAKE AFTER A MUSCLE TEAR
Our muscles play an important role in the movement of our body. Without our muscles, we wouldn’t be able to bend our elbow or straighten our leg. As our muscles are soft and designed for flexibility, they are also prone to injury and if you have ever had a muscle tear, you know that they can be surprisingly painful.
In the period following a muscle tear, there are a few mistakes we see people make, that can actually make their injury worse and delay healing times. Here are a few of the most common mistakes we see.
1. Stretching
After a muscle tear, the damaged fibres slowly begin to heal and reattach to each other. This process can be quite fragile and during the early stages, aggressive stretching of recovering tissue can impair healing or even lead to more tearing. While gentle stretching a few days after the injury can have a positive effect, you should check with your physiotherapist to ensure you’re not stretching too far and causing further damage.
2. Applying H.A.R.M.
Most of us are aware of the acronym R.I.C.E (rest, apply ice, compress the area and elev
ate) as the recommended treatment in the early stages of an acute injury. The acronym H.A.R.M is less well known and is used to remember the things you shouldn’t do after an injury. This stands for applying heat, drinking alcohol, running or massage. All of these activities can increase swelling, pain and increase the damage of the injury in the first 48-72 hours.
3. Failing to see a physiotherapist
The diagnosis of a muscle tear might seem straightforward, however, there might be more going on than you realize. Many conditions can mimic a muscle tear, or you may have suffered a tear due to an underlying weakness or pathology. Having a physiotherapist confirm your muscle tear or identify another condition is vital to ensuring you recover fully.
Your physiotherapist is also able to identify any factors that could lead to further injury and is able to help restore your tissue to its previous level.
4. Returning to sport too early
One of the most confusing things about muscle tears is that often they become less painful while the tissues are still not completely healed. Many people suffer another tear simply because they return to sport too early. While you may feel as though your tissues are back to full strength, the muscle fibres can still be healing and vulnerable to a tear. It is important to test your injury gradually, starting with gentle exercise and building up to high-intensity activities.

Most tissues in the body have healed completely in six to 12 weeks following an injury, however, many people have severe pain that lasts much longer than this. We know that the intensity of the pain you feel is not always associated with a similar amount of damage. In some cases, there can be a severe amount of pain with almost no detectable damage. With this in mind, we explore some reasons why your pain might not be getting better, long after the tissues have healed. You’re afraid of the pain. Pain can mean many different things, for some of us pain can affect our ability to work or can be a symptom of a serious disease. What you believe about your pain can either amplify or reduce the symptoms you experience. If you feel that every time you experience pain you are causing more damage, you will naturally pay more attention to this and your nervous system will amplify the signals in an attempt to keep you safe. If you understand the cause of your pain and know that while there is discomfort, you are not in danger of causing more damage, often the pain will feel less severe. This is one of the benefits of seeing a physiotherapist after your injury as they can help you to understand your pain, giving you more control over your recovery. You started moving differently after the injury. Immediately after an injury, it’s natural to change the way you move to avoid painful movements. After a while, these changed movement patterns can become maladaptive and actually begin to cause pain and discomfort on their own due to the altered stress patterns placed on your body. Correcting these adaptive movement patterns can often go a long way in reducing pain after an injury. You might not have noticed these changes and might need a physiotherapist to identify and help you to return to your usual movement pattern. You have lost muscle strength since the injury. While a certain amount of rest following an injury is always helpful, if we stop moving altogether, our muscles can lose strength. This can mean that our posture changes, we fatigue easier during our usual activities and that we are more susceptible to further injury. Less movement also means we actually focus on the pain more when it does happen. Physiotherapists are able to advise you on the right types and amounts of excercise for you in the period following your injury. The pain has affected your lifestyle. When pain affects your ability to sleep, work and even concentrate, it’s not surprising that this can have a negative affect on your overall wellbeing and mental health. This can create a negative cycle of anxitey and depression that perpetuates and increases the experience of pain. If your pain is really getting you down, speaking to a mental health professional can actually be a valuable part of your physical recovery

What is spinal stenosis? The spinal cord, nerves and arteries are housed by the spine, which acts as a hard electrical casing to support and protect these vulnerable structures. The spine has a hollow column that allows the spinal cord to run from the brain to the rest of the body. At each spinal segment, nerves exit the spine and supply the tissues of the body. There is also an intricate network of small veins and arteries that provide blood to the spinal cord and vertebrae, providing them with the nutrients needed to operate. Spinal stenosis is characterized by a narrowing of the spaces that house the spinal cord, nerves and blood supply. A variety of factors can cause spinal stenosis, however overwhelmingly it is caused by degenerative changes to the spine as we age. Many people over the age of 60 will have spinal stenosis; however, not all will have pain. Clinically, spinal stenosis is used to describe the painful symptoms of this condition rather than just the narrowing itself.

What is it? When the two surfaces of the hip joint move over each other, they usually move freely without any friction. If there is an alteration to either the socket part of the joint (the acetabulum) or the ball (the head of the femur), irritation may occur as the two surfaces move over each other. This is known as Femoroacetabular impingement, a common disorder of the hip, characterized by pain and stiffness. Femoroacetabular impingement can be classified as cam, pincer or mixed. A cam FAI occurs when the femoral head junction is flattened or a small bump is present. Pincer type of impingement occurs when the acetabular rim extends slightly, causing the femur to be impacted. Cam impingement is more common in men while pincer impingement is more common in women. However, most cases of FAI (about 85%) are mixed, meaning they both have cam and pincer types of impingement.

Ankle sprains are one of the most common sporting injuries and most people have experienced one at least once in their lifetime. While they are common, this doesn’t lessen their negative impacts. Surprisingly, having poor balance might be increasing your risk of ankle sprains. Here we discuss a few facts about balance and what you can do to reduce your risk of ankle injuries.

What Are They? Muscular trigger points are better known to most of us as muscle knots and can feel like painful, hard lumps located inside muscles. These knots can both be painful to touch and refer pain in surrounding areas. It is thought that trigger points form when a portion of muscle contracts abnormally, compressing the blood supply to this area, which, in turn, causes this part of the muscle to become extra sensitive. Trigger points are a common source of pain around the neck, shoulders, hips and lower back.

When injury strikes, the first thing that most of us want to know is ‘how long will this take to heal?’ Unfortunately, the answer to this can be complicated and requires at least a little understanding of how the different tissues of the body heal. Each of the tissues of the body, including muscles, tendons, ligaments and bone, heal at different speeds and each individual will have some variation on those times as a result of their individual health history and circumstances.