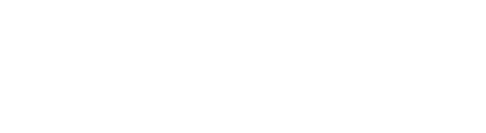
The Causes of Mid Back Pain

Mid Back Pain (or thoracic pain) is one of the most common conditions we treat. The causes are many and varied (as listed below) yet they almost all respond to Physiotherapy well.
Pain in the mid back can be sudden or gradual. Sudden onset thoracic pain often occurs via a sort of trauma - contact sports, motor vehicle accidents, heavy lifting, bending forward or sideways or twisting. Mid back pain can commonly be referred pain from an issue in your neck.
Gradual onset mid back pain often occurs from low level, persistent, stress to osseo-ligamentous structures in your mid back. This occurs in people that sit for long periods for work or study, especially from prolonged slouching. In older patients with gradual onset mid back pain, one of the most likely causes of symptoms is a flare up of degenerative changes in the spine (Arthritis).
Common causes of mid back pain
- Prolonged or repetitive (poor) postures (Postural Syndrome)
- Referred pain from your cervical spine (neck)
- Muscle fatigue, strain, overactivity
- Degenerative disc disease
- Herniated disc (disk bulge)
- Thoracic spondylosis
- Facet joint loading and subsequent muscle tightness or spasm
Top 5 Tips to Reduce Your Mid Back Pain!
Avoid or modify known aggravating activities - This doesn’t mean stop doing everything – just be mindful of the way you do certain activities like twisting around in the car. If you feel looking at your phone or at your computer screen brings on your pain, then you will have to minimise your time doing this to let your back recover quickly.
Correct your posture – A correct posture takes physical load off components in your mid back including vertebrae, disks and muscles. It is important to be mindful of not just sitting posture but also standing and bending postures. It is also important to be aware of your posture throughout the day, especially in the evenings when people are often a bit tired and start to slouch. It is good practice to set up reminders for yourself. It is vital for a good long term result that posture is corrected and stays corrected. This will prevent recurrence. Specific stretching and strengthening exercises can also help to improve posture and activity tolerance.
Stretch – Gently but frequently. Don’t worry if you can’t move very far before you feel stretch to start with, your movement will improve gradually. Your neck, mid back and Pecs (chest) are the most important. Hold stretches for 20 – 30 seconds at a point of stretch feeling or discomfort – never pain.
Apply Heat / Cold pack – Don’t underestimate how much pain relief these can give you. Your Physio can advise which is the most appropriate and helpful in your particular circumstance. Heat is generally for loosening tight and spasmed muscles. Cold can help reduce pain and inflammation from a trauma type incident.
Self-mobilise joints – This loosening of the joints in your mid back is safe and takes pressure off your spine. Applying a heat pack before you perform this helps loosen the muscles around the joints and can give an even better result. Ways to do this include laying on devices like a posture pro, back balls or foam roller. These are available at our clinic – talk to the team for what will be best for your circumstance.
We CAN Help! Your Physio at OFP will be able to determine the likely cause of your mid back pain. Most patients will recover fully from a short course of physiotherapy.
Call one of our friendly staff today on
3470 1203 to experience healthcare that cares and get that mid back pain gone!